Reasons You Might Have an Ingrown Toenail
 An ingrown toenail occurs when the outer edge of a toenail grows into the surrounding skin, rather than over it. This causes redness, swelling, pain, and inflammation around the ingrown toenail. The area is also at an increased risk of infection. Several factors make an ingrown toenail more likely to develop. Trimming the toenails improperly, by cutting them too short or into a rounded shape, makes the skin more likely to fold over the nail. Wearing shoes that are too tight or narrow in the toe area can squish the nails into the skin. Having excessively sweaty feet can make the skin surrounding the nails too soft, allowing the nail to pierce through the skin more easily. Sometimes an injury to the toenail can cause an ingrown nail to develop. Some people also have nails that naturally grow in a curved or fan-like shape that can make ingrown nails more likely. If you have a painful or infected ingrown toenail, or if you are prone to ingrown toenails, it is suggested that you seek the care of a podiatrist.
An ingrown toenail occurs when the outer edge of a toenail grows into the surrounding skin, rather than over it. This causes redness, swelling, pain, and inflammation around the ingrown toenail. The area is also at an increased risk of infection. Several factors make an ingrown toenail more likely to develop. Trimming the toenails improperly, by cutting them too short or into a rounded shape, makes the skin more likely to fold over the nail. Wearing shoes that are too tight or narrow in the toe area can squish the nails into the skin. Having excessively sweaty feet can make the skin surrounding the nails too soft, allowing the nail to pierce through the skin more easily. Sometimes an injury to the toenail can cause an ingrown nail to develop. Some people also have nails that naturally grow in a curved or fan-like shape that can make ingrown nails more likely. If you have a painful or infected ingrown toenail, or if you are prone to ingrown toenails, it is suggested that you seek the care of a podiatrist.
Ingrown toenails may initially present themselves as a minor discomfort, but they may progress into an infection in the skin without proper treatment. For more information about ingrown toenails, contact Jon McCreary, DPM of Fort Worth Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails are caused when the corner or side of a toenail grows into the soft flesh surrounding it. They often result in redness, swelling, pain, and in some cases, infection. This condition typically affects the big toe and may recur if it is not treated properly.
Causes
- Improper toenail trimming
- Genetics
- Improper shoe fitting
- Injury from pedicures or nail picking
- Abnormal gait
- Poor hygiene
You are more likely to develop an ingrown toenail if you are obese, have diabetes, arthritis, or have any fungal infection in your nails. Additionally, people who have foot or toe deformities are at a higher risk of developing an ingrown toenail.
Symptoms
Some symptoms of ingrown toenails are redness, swelling, and pain. In rare cases, there may be a yellowish drainage coming from the nail.
Treatment
Ignoring an ingrown toenail can have serious complications. Infections of the nail border can progress to a deeper soft-tissue infection, which can then turn into a bone infection. You should always speak with your podiatrist if you suspect you have an ingrown toenail, especially if you have diabetes or poor circulation.
If you have any questions, please feel free to contact our office located in Fort Worth, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Ingrown Toenail Care
An ingrown toenail is a nail that has curved downward and grows into the skin. This typically occurs at the nail borders, or the sides of the nail. As a result, pain, redness, swelling, and warmth may occur in the toe. If a break in the skin forms due to the ingrown nail, bacteria may enter and cause an infection in the area; this is typically characterized by a foul odor and drainage.
Ingrown toenails have multiple reasons for developing. In many instances, the condition is a result of genetics and is inherited. The most common cause, however, is improper trimming; cutting the toenails too short forces the skin beside the nail to fold over. An ingrown toenail can also develop due to trauma, such as stubbing the toe, having an object fall on the toe, or participating in activities that involve repeated kicking or running. Wearing shoes that are too tight or too short can also cause ingrown toenails.
Treatment for an ingrown toenail varies between patients and the severity of the condition. Milder cases that don’t involve infection or other medical conditions can benefit from soaking the feet in room-temperature water and gently massaging the side of the nail. In most cases, however, it is best to see your podiatrist for thorough and proper treatment. After examining your toe, your podiatrist may prescribe oral antibiotics to clear the infection if one is present. Surgical removal of either a portion of the nail or the entire nail may also be considered. In some cases, complete removal or destruction of the nail root may be required. Most patients who undergo nail surgery experience minimal pain afterward and can return to normal activity the following day.
Ingrown toenails can be prevented with proper nail trimming and by avoiding improper-fitting shoes. When cutting the toenails, be sure that you are cutting in a straight line and avoid cutting them too short. Shoes should not be too short or tight in the toe box.
Tarsal Tunnel Syndrome and Rheumatoid Arthritis
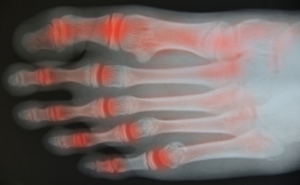
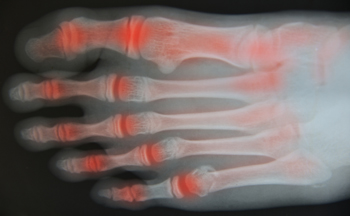 Rheumatoid arthritis (RA) is an autoimmune disease in which the body’s immune system attacks the otherwise healthy cells that make up the linings of joints. Because each foot contains 33 joints, the feet, as well as the ankles, are often affected. RA can make other foot and ankle conditions more likely to occur. One such condition is tarsal tunnel syndrome, in which the posterior tibial nerve is compressed or damaged, causing burning pain, numbness, and tingling in the affected foot. Tarsal tunnel syndrome is frequently seen in people with RA. If you have RA, it is suggested that you be under the care of a podiatrist who can monitor the health of your feet and treat any problems as they arise.
Rheumatoid arthritis (RA) is an autoimmune disease in which the body’s immune system attacks the otherwise healthy cells that make up the linings of joints. Because each foot contains 33 joints, the feet, as well as the ankles, are often affected. RA can make other foot and ankle conditions more likely to occur. One such condition is tarsal tunnel syndrome, in which the posterior tibial nerve is compressed or damaged, causing burning pain, numbness, and tingling in the affected foot. Tarsal tunnel syndrome is frequently seen in people with RA. If you have RA, it is suggested that you be under the care of a podiatrist who can monitor the health of your feet and treat any problems as they arise.
Because RA affects more than just your joints, including the joints in your feet and ankles, it is important to seek early diagnosis from your podiatrist if you feel like the pain in your feet might be caused by RA. For more information, contact Jon McCreary, DPM of Fort Worth Podiatry. Our doctor will assist you with all of your podiatric concerns.
What Is Rheumatoid Arthritis?
Rheumatoid Arthritis (RA) is an autoimmune disorder in which the body’s own immune system attacks the membranes surrounding the joints. Inflammation of the lining and eventually the destruction of the joint’s cartilage and bone occur, causing severe pain and immobility.
Rheumatoid Arthritis of the Feet
Although RA usually attacks multiple bones and joints throughout the entire body, almost 90 percent of cases result in pain in the foot or ankle area.
Symptoms
- Swelling and pain in the feet
- Stiffness in the feet
- Pain on the ball or sole of feet
- Joint shift and deformation
Diagnosis
Quick diagnosis of RA in the feet is important so that the podiatrist can treat the area effectively. Your doctor will ask you about your medical history, occupation, and lifestyle to determine the origin of the condition. Rheumatoid Factor tests help to determine if someone is affected by the disease.
If you have any questions please feel free to contact our office located in Fort Worth, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Rheumatoid Arthritis in the Feet
Although rheumatoid arthritis attacks multiple bones and joints throughout the entire body, ninety percent of people who actually develop this condition usually do so in the foot or ankle area. Those who develop this kind of arthritis in the feet usually develop symptoms around the toes and forefeet first, before anywhere else. Rheumatoid arthritis appears to have a genetic component. If it runs in the family, then you will be more likely to develop it as well.
Rheumatoid arthritis is an autoimmune disorder in which the body’s own immune system attacks the lining of the membranes surrounding the joints. This causes inflammation of the membrane lining, and the gradual destruction of the joint’s cartilage and even bone.
Some of the most common symptoms that are associated with RA include pain and swelling of the feet. Stiffness in the feet is also another common symptom that people experience. Those who have RA in the feet usually feel the pain in the ball or sole of their feet. This can get to be very painful at times. A person's joints can even shift and become deformed after a period of time.
In order to properly diagnose RA in the feet it is usually necessary for a doctor or podiatrist to evaluate the area. Your doctor will also question you about your medical history, occupation, etc., to determine whether anything in your lifestyle may have triggered the condition. There are a number of tests that may be performed to help diagnose RA, such as a rheumatoid factor test. There is, however, no one single test that will tell you for sure if you have RA. There are different X-rays that can be taken as well to determine if a person has RA in their feet.
There is a range of treatment options for rheumatoid arthritis. Treatment of RA is usually a lifelong process that includes a variety of methods of treatment and therapy. Your doctor can prescribe special shoes that should help with arch support as well as heel support. A physical therapist can help those with this condition learn exercises which will keep their joints flexible. Surgery may be needed to correct some of the issues with the feet, such as bunions, and hammertoes. Fusion is usually the most successful surgical option for rheumatoid arthritis. However, people need to keep in mind that there are some risks associated with these surgeries.
Are Bunions Affecting Your Everyday Life?
Foot Pain Caused by Sciatica
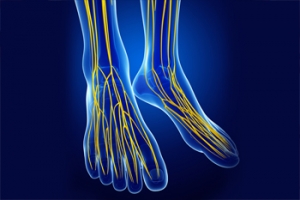
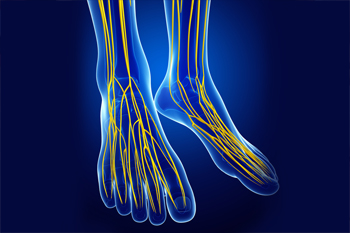
The sciatic nerve is the body’s largest nerve. It runs from the lower back to the knees before branching into other nerves that extend to the feet and toes. When this nerve becomes pressured or compressed, it causes a condition known as sciatica which can cause radiating or electric pain starting in the lower back down to the toes. There may even be feelings of tingling or numbness. The many possible causes of sciatica include a herniated disc, a narrowing of the spinal column due to age (spinal stenosis), bad posture, trauma, nerve disorders, muscular strain, being overweight, and vertebral misalignment. Sciatica usually affects people aged 40 and older. Those who work in awkward positions are believed to be more at risk of developing sciatica. If you believe you may have sciatica, it’s wise to contact a podiatrist for a proper diagnosis. Treatment to relieve pressure on the sciatic nerve may include massage and/or physical therapy, stretching, medication, biomechanical adjustments with orthotics, or possibly even surgery, depending on the cause.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with Jon McCreary, DPM from Fort Worth Podiatry. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our office located in Fort Worth, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot Pain
Our feet are arguably the most important parts of our bodies because they are responsible for getting us from place to place. However, we often don’t think about our feet until they begin to hurt. If you have pain in your feet, you need to first determine where on the foot you are experiencing it to get to the root of the problem. The most common areas to feel pain on the foot are the heel and the ankle.
Heel pain is most commonly attributed to a condition called plantar fasciitis. Plantar fasciitis occurs when the plantar fascia, which is the band of tough tissue connecting the heel bone to the toes becomes inflamed. Plantar fasciitis pain is usually worse in the morning, and it tends to go away throughout the day. If you have plantar fasciitis, you should rest your foot and do heel and foot muscles stretches. Wearing shoes with proper arch support and a cushioned sole has also been proven to be beneficial.
Some common symptoms of foot pain are redness, swelling, and stiffness. Foot pain can be dull or sharp depending on its underlying cause. Toe pain can also occur, and it is usually caused by gout, bunions, hammertoes, ingrown toenails, sprains, fractures, and corns.
If you have severe pain in your feet, you should immediately seek assistance from your podiatrist for treatment. Depending on the cause of your pain, your podiatrist may give you a variety of treatment options.
Flexible Flat Feet in Children
 It is not unusual for a child to have a condition known as flexible flat feet. Symptoms include a flattened arch, which results in the feet splaying outward. This may cause some pain in the arch if the child is particularly active. Avoiding weight-bearing activities, such as running, and turning instead to cycling or swimming, can give the heels a rest. Stretching the outer calf muscles on a daily basis can also help. Wearing shoes with cushioning and support as well as a slight heel can help to decrease pounding on the heel and the flattening of the arch. Custom orthotics can also be used to help eliminate discomfort. A podiatrist can perform tests to determine the severity of the case and suggest several remedies to reduce the symptoms. It is a good idea to plan regular visits to allow the doctor to monitor your child’s foot condition on a regular basis.
It is not unusual for a child to have a condition known as flexible flat feet. Symptoms include a flattened arch, which results in the feet splaying outward. This may cause some pain in the arch if the child is particularly active. Avoiding weight-bearing activities, such as running, and turning instead to cycling or swimming, can give the heels a rest. Stretching the outer calf muscles on a daily basis can also help. Wearing shoes with cushioning and support as well as a slight heel can help to decrease pounding on the heel and the flattening of the arch. Custom orthotics can also be used to help eliminate discomfort. A podiatrist can perform tests to determine the severity of the case and suggest several remedies to reduce the symptoms. It is a good idea to plan regular visits to allow the doctor to monitor your child’s foot condition on a regular basis.
Flatfoot is a condition many people suffer from. If you have flat feet, contact Jon McCreary, DPM from Fort Worth Podiatry. Our doctor will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact our office located in Fort Worth, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What is Flexible Flat Foot?
Flatfoot is classified as having the entire sole of the foot in contact or near contact to the ground while standing. The disorder is also known as fallen arches, because those affected have no arch in their feet. Flexible flatfoot and rigid flatfoot are the two types of flatfoot.
A person has flexible flatfoot if when sitting or standing on their toes, they have an arch that disappears when they stand with the entire foot on the ground. Flexible flatfoot may also be called “pediatric flatfoot” because the condition first appears in childhood. It is common among infants because the arch does not develop until the age of 5 or 6 years. Rigid flatfoot is not as common in children as it is with adults. This type of flatfoot is developed due to the weakening of tibialis posterior muscle tendon, a major supporting structure of the foot arch. Development of this deformity is progressive and shows early signs of pain and swelling that begins at the inside arch of the foot and moves to the outside of the foot below the ankle. More severe cases can possibly lead to arthritis of the foot and ankle joints.
Although most cases of flatfoot involve people born with the condition, some less common causes are obesity, diabetes, pregnancy, and osteoporosis. In some cases, flatfoot may come with no symptoms at all and does not require any type of treatment. With other cases though, symptoms may include pain in the shin, knee, hips and lower back. If a person with flatfeet experiences such symptoms, a health care provider may suggest using orthotic devices or arch supports, which may reduce the pain. Wearing supportive shoes can also prove more comfortable with flatfeet and staying away from shoes with little support such as sandals. Other methods to relieve pain also include stretching the Achilles tendon properly and using proper form when doing any physical activity. In addition, losing weight can reduce the stress on your feet and reduce the pain.
Vascular Testing to Help Determine Peripheral Arterial Disease
Some of the symptoms of peripheral arterial disease (PAD) can include pain, weakness, numbness, loss of hair on your legs, bluish-colored skin on the feet or calves, poor toenail growth, pain or cramps in your legs when walking, and wounds on your feet and legs that are slow to heal. To properly diagnose this vascular condition, your podiatrist may need to know your Ankle Brachial Index (ABI). Simply put, the ABI compares the blood pressure in the arm with the blood pressure in the ankle. Blood pressure during the heart’s contracting/pumping (systolic) phase is slightly higher in the ankle than it is in the arm for healthy people. Determining the ABI is a very simple and non-invasive procedure, using just a blood pressure cuff and a Doppler instrument. The patient lies down and rests for ten minutes. Then, blood pressure is taken at the upper arm, followed by the ankle. The ankle’s blood pressure is then divided by the arm’s blood pressure. An ABI ratio between 1.0 to 1.4 is considered normal. An ABI ratio of 0.9 or less usually indicates PAD—with moderate cases typically ranging between 0.4 to 0.7, and more severe cases falling below 0.4. If you are experiencing any symptoms of PAD, contact a podiatrist right away for a full examination and to see if your ABI should be analyzed.
Vascular testing plays an important part in diagnosing disease like peripheral artery disease. If you have symptoms of peripheral artery disease, or diabetes, consult with Jon McCreary, DPM from Fort Worth Podiatry. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Vascular Testing?
Vascular testing checks for how well blood circulation is in the veins and arteries. This is most often done to determine and treat a patient for peripheral artery disease (PAD), stroke, and aneurysms. Podiatrists utilize vascular testing when a patient has symptoms of PAD or if they believe they might. If a patient has diabetes, a podiatrist may determine a vascular test to be prudent to check for poor blood circulation.
How Is it Conducted?
Most forms of vascular testing are non-invasive. Podiatrists will first conduct a visual inspection for any wounds, discoloration, and any abnormal signs prior to a vascular test.
The most common tests include:
- Ankle-Brachial Index (ABI) examination
- Doppler examination
- Pedal pulses
These tests are safe, painless, and easy to do. Once finished, the podiatrist can then provide a diagnosis and the best course for treatment.
If you have any questions, please feel free to contact our office located in Fort Worth, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.